Anatomy
The breasts are paired mammary glands composed of hormone responsive fibro glandular tissue and fat contained in a skin envelope. The breasts sit on the chest wall, extending from the 2nd rib above to the 6th rib below and into the armpit (the axillary tail).
Breasts come in all shapes and sizes and are not always symmetrical. The ratio of glandular and adipose tissue determines the density (or firmness) of the breast. It is important that women who have dense breasts are educated about this, as it may impact on the sensitivity of breast screening. Furthermore, increased breast density is an independent risk factor for breast cancer.
In females the primary physiological function of breasts is to breastfeed. However, for many women they are also important to their sense of self, body image and sexual attractiveness. It is crucial that all of these attributes are considered in the treatment of women with breast problems.
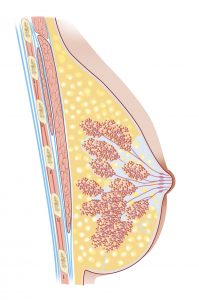
Cross-section of the female breast showing fibroglandular and adipose tissue.
Breast Development
Both men and women develop breast from the same embryological tissues. They undergo multiple changes in form and function as we develop, from birth, puberty, pregnancy, lactation and menopause. In males, the breasts remain rudimentary in their pre pubertal state. Occasionally, gynaecomastia or enlargement of the breasts can occur and may be due to hormonal causes or medications.
Breast Awareness
An important measure in maintaining the health of your breasts and detecting any changes is simply knowing what is normal for you. Knowing the normal appearance, feel, texture and shape of your breasts, particularly at different stages of the menstrual cycle, assists in identifying abnormal changes. This is commonly referred to as breast awareness. Showering, lying in bed or whilst get ting dressed can all be ideal times to self-examine and should be performed by women of all ages.
Benign breast abnormalities
Accessory breast tissue (polymastia).
This is a developmental variation whereby abnormal breast tissue is found in addition to the normal breasts. It is often not detected until puberty.
Accessory breast tissue can be found anywhere along the “mammary lines”, extending from the armpits to the normal chest nipples, and downwards to the groin or inner thigh. Breast cancer can rarely occur in accessory breast tissue. Symptomatic accessory breast tissue can be removed surgically if required.
Third nipple
This is an accessory, or supernumerary, nipple and is a common variation of normal development in both men and women. They very rarely develop with an areola and breast tissue and are difficult to detect to an untrained eye. Accessory nipples can be removed for cosmetic reasons or if symptomatic. There is no association with breast cancer.
Breast Lumps
The majority of lumps are be benign, particularly in younger women (>90%), however it is critical to assess each lump in the same way. All breast lumps should be examined by a doctor and ideally a breast specialist, followed by imaging and in most cases a biopsy. This is called triple assessment. There are many causes of breast lumps including benign and malignant pathologies. Importantly, not all breast problems can be palpated (i.e. felt) but they are seen on imaging.
a) Localised nodularity
This is a common finding, particularly in young women, and is a reflection of normal physiological changes throughout the menstrual cycle. Clinical monitoring for 2-3 months is typically sufficient for a cyclical and symmetrical nodularity in younger women. If there are any suspicious features, triple assessment is recommended.
b) Breast cysts
Breast cysts are fluid-filled cavities, which occur when the amount of fluid normally secreted by the milk ducts is greater than the amount absorbed. Breast cysts are a very common finding on mammograms or ultrasounds, particularly in women aged 30-50 years (but they can occur in women of any age). It is normal for breast cysts to vary in size at different stages of the menstrual cycle, or to regress completely. On examination breast cysts are smooth and distinct from the surrounding breast tissue. They are often mobile and tender, especially if the fluid is under pressure. Breast cysts are benign and have no malignant potential. In extremely rare cases, a cyst may harbour a cancer (intra-cystic carcinoma) but these cysts are atypical in many ways. The decision of whether or not to treat a lump that has features of a typical, well-defined cyst is partly dependent on the woman’s preferences. Small cysts generally are not palpable, and do not require treatment. Larger cysts can be aspirated (the fluid is sucked out with a needle). Surgery is not typically recommended unless the cysts are recurrent after repeated drainage or if there are any worrying features.
c) Fibroadenomas
Fibroadenomas are a very common benign breast condition. They represent an overgrowth of normal tissue supporting the breast tissue. Fibroadenomas are most common in young women. On examination they are classically smooth, rubbery and mobile. Diagnosis is confirmed by biopsy. If the lesion is too small to biopsy and looks typical of a fibroadenoma on ultrasound, follow up ultrasounds may be recommended instead. The management of a fibroadenoma is usually conservative (no surgery) but in some instances surgery may be recommended eg. patient preference increases in size over time, larger than 5cm or it is painful.
d) Fat necrosis
Trauma to the breast can produce an area of fat necrosis (dead fat) that presents like a lump. This will typically feel firm and non-painful and the surrounding skin may look red, bruised, dimpled or entirely normal. While it is benign, biopsy is always recommended as examination and imaging share many characteristics with cancer. There is no associated risk of breast cancer with fat necrosis. In some circumstances surgical removal may be suggested to exclude cancer.
e) Breast cancer
See below
Breast pain (Mastalgia)
Breast pain affects about 70% of women at some point in their lives. Breast pain is not typically a sign of breast cancer. Most commonly, no specific cause is identified. There are two main categories of breast pain; cyclical and non-cyclical.
a) Cyclical Breast Pain
This is more common and generally occurs in pre-menopausal women. It often affects the upper outer quadrants of both breasts (bilateral), though may be felt more strongly on one side. It usually occurs in the week leading up to each period and settles with menstruation.
b) Non-Cyclical Breast Pain
This is less common and does not vary with the menstrual cycle. It is more prevalent in older women. Non-cyclical breast pain is often restricted to one breast (unilateral) and is localised to a particular part of the breast
A third pseudo-subtype of breast pain is called extra-mammary pain and actually has no relation to the breast at all. This pain is caused by the muscles, ligaments and ribs that make up the chest wall. Extramammary breast pain may be triggered by physical exercise.
It is important to exclude a structural cause for the pain. Once this is established, for many women, reassurance that their pain is not due to cancer is enough and no further treatment is required. For others the severity of pain is debilitating, and intense management is needed. Options range from supportive measures like a well-fitting bra, to dietary supplements such as evening primrose oil (1000mg four times a day for 3-6months), to simple analgesia (eg. Panadol) and hormonal therapies (eg. oral contraceptive pill or tamoxifen for very severe cases). Severe breast pain should ultimately be managed by a breast specialist.
Skin changes associated with breast disease
Skin changes can be particularly prominent in some types of breast cancer, but most often are not relevant. It is important to be assessed by a breast specialist if you are concerned about any skin changes.
a) Skin puckering or dimpling
This is caused by scar tissue forming in the breast. A specific type of dimpling known as ‘peau d’orange’ is associated with breast cancer. In this condition the skin overlying the breast resembles orange peel (peau) due to infiltration of cancer cells in the small ligaments supporting the breast.
b) Warmth and redness
Breast infections are common in lactating women, especially new mothers. Cracked nipples act as a portal for bacterial entry which then proliferate and cause mastitis. Mastitis is extremely painful and can cause serious systemic illness if left untreated. An ultrasound is necessary to exclude a breast abscess. Treatment involves massage, continued breastfeeding (or pumping) and broad-spectrum antibiotics.
c) Itchiness, flaking and scaly skin
Crusty or scaly skin can be a sign of infection or often eczema. When associated with the nipple, it may be a sign of Paget’s disease. Prompt consultation with a breast specialist is very important.
Nipple Changes
Inversion People can can be born with inverted nipples, where the nipples indent inwards although on stimulation, they will generally face outwards. This is completely normal and does not require assessment by a doctor. Nipple retraction or inversion that is new, occurring only in one breast, or where the nipple does not come out on stimulation can be a concerning sign of breast cancer. This should be immediately reviewed.
Paget’s disease
This is a very rare form of breast cancer. The nipple appears scaly, raw or ulcerated. Many patients describe nipple pain or a burning sensation that preceded the appearance of the rash. It is crucial never to dismiss nipple rash. Triple assessment and punch biopsy of the skin is necessary.
Nipple discharge
Spontaneous nipple discharge is very common. It can be physiological or pathological and associated with both benign and malignant pathology. The most concerning nipple discharge is spontaneous, single duct, unilateral and persistent. The consistency and colour of the discharge does not decrease the suspicion for breast cancer. Approximately half of the patients that present with nipple discharge will also have a breast lump but only one in 5 of these patients will have a breast cancer. Investigation of a patient with nipple discharge includes triple assessment and at times ductography.
There are several potential causes:
- Mammary Duct Ectasia– is most common is older smokers. The ducts are irregularly dilated and filled with secretions (ectatic)
- Intraductal papilloma– is a small growth (wart-like lesion) within the milk duct usually within 2 cm of the nipple. It can be asymptomatic, or it can be associated with a nipple discharge. It usually comes from a single duct and is usually unilateral. In less than 10% of cases, a papilloma can be associated with cancer and surgical excision is necessary.
- Dermatitis may affect the skin of the nipple and cause a pseudo-discharge (weeping). Short term cortisone-based cream is the first line of treatment, but it is important that the problem is properly investigated (to exclude Paget disease).
- Galactorrhoea this is a milky, usually bilateral, nipple discharge which is not related to pregnancy or breastfeeding. It occurs when the pituitary gland causes the abnormal production of prolactin. Prolactin is a hormone that stimulates milk production. Some medications can also cause galactorrhoea such as antidepressants, antipsychotics, cocaine and opioids.
- Breast Cancer approximately 5% of women with breast cancer will have nipple discharge. The discharge associated with breast cancer may be bloody, clear or serosanguinous. In other words, colour is not sensitive.
Surgery for nipple discharge is either microdochectomy (single duct excision) or a central duct excision (multiple ducts).
High Risk Breast Lesions
A high-risk breast lesion refers to a lesion that is associated with an increased risk of developing future breast cancer or has a more concerning underlying pathology. While these lesions are not breast cancer per se, excision is often recommended.
Sclerosing adenosis, is a special type of adenosis where scar tissue forms within the enlarged lobules and distorts them. There is an associated increased risk for developing breast cancer in future, x1.5-2.
Atypical ductal hyperplasia (ADH) this is a pathological term that describes the appearance of atypical cells in the milk ducts under a microscope. There is an overgrowth of the cells lining the milk ducts of the breast which show abnormal cellular characteristics. The risk of developing breast cancer in the future is approximately 10% within 10 years. risk of contralateral breast cancer is also increased.
Atypical lobular hyperplasia (ALH) this refers to an overgrowth of the cells within the lobules (milk-producing glandular tissue) of the breast which show abnormal characteristics. It is a mild breast lesion that is associated with an increased risk of future development of breast cancer, x4-6. Often it is an incidental finding on a surgical specimen and no further treatment is required other than regular monitoring.
Lobular carcinoma in situ (LCIS) this occurs when abnormal cells are contained within the lobules of the breast but do not extend beyond the terminal duct. Women who develop LCIS have an increased risk of developing breast cancer in the future, although that is still uncommon. Monitoring, rather than treatment, is usually all that is needed.
Radial scar/Complex sclerosing lesion Despite the name this is not related to scar tissue. Its significance is in its ability to mimic the appearance of breast cancer on mammography and therefore is often excised. It has a mild association with DCIS and some invasive tumours.
Breast Cancer
Breast cancer is an increasing public health problem. There have been substantial advances made in treatment of breast cancer however the incidence is rising in most countries despite vigorous advancements in treatment.
Accepted risk factors for breast cancer are younger age of menarche (age of first period), older age of first pregnancy, fewer pregnancies, shorter or no periods of breastfeeding, and later menopause. Other risk factors include physical inactivity, hormone replacement therapy, increased alcohol consumption and obesity. The impact of hereditary breast cancer has also increased. In Victoria, breast cancer is the most common new cancer diagnosis with almost 4075 diagnoses in 2013 (almost 30% of all cancers).
Breast cancer can present with a variety of symptoms. These may include a breast lump, breast thickening, nipple discharge and changes to the skin overlying the breast or the nipple. It may also present with changes in the contour or shape of the breast, a lump under the armpit or breast pain. In many cases breast cancer may be totally asymptomatic and found on routine breast imaging.
It is recommended that women between the ages of 50 and 74 undergo screening mammograms with BreastScreen every two years. Younger women aged 40 to 49 are also covered by the programme and are welcome to attend. Women with a higher risk of developing breast cancer may be eligible for additional screening such as breast MRI. This can be discussed with Dr Edwina during your consultation.
One third of all women who have dense breasts will maintain this density in the post menopause.
Ductal carcinoma in situ (DCIS)
This is the most common form of non-invasive breast cancer and refers to abnormal cells that are confined to the milk ducts of the breast. “In situ” refers to the cancer being restricted to its original site; that is, it has not invaded the tissue surrounding the milk duct. DCIS does not generally present as a palpable lump and instead is found on mammography as atypical calcification A core biopsy is recommended in order to provide a clear diagnosis. The treatment of DCIS is surgery with a 2mm margin of normal breast tissue. This may be either a lumpectomy (with radiotherapy) or mastectomy, depending on the size of the DCIS and the breast. DCIS increases the risk of invasive cancer.
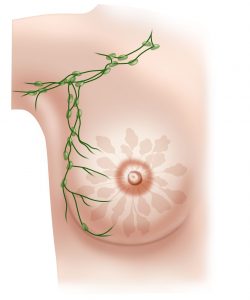
Breast cancer can spread to the lymph nodes in the armpit. A sentinel lymph node biopsy is a diagnostic test (done in the operating room under general anaesthetic as part of your breast cancer surgery), to assess whether the cancer has spread to the nodes.
Ductal carcinoma
This is the most common type of invasive breast cancer and arises from the epithelium lining the ducts within the breast. Risk factors for breast cancer are female gender, obesity, a sedentary lifestyle, estrogen exposure (timing of menarche, menopause, number of pregnancies, breastfeeding, use of HRT) and family history. About 5-10% of breast cancers are due to breast cancer genes eg. BRACA1 and BRACA2. Diagnosis of breast cancer is made via a core biopsy, which typically follows either an abnormal imaging results or clinical finding (eg. a lump, skin or nipple change). A number of treatments may be used, including surgery, radiation therapy, chemotherapy, hormonal therapy, and targeted therapy. Types of surgery vary from breast-conserving surgery to mastectomy. Breast reconstruction may take place at the time of surgery or at a later date. In addition, it is necessary to examine whether the cancer has spread to regional axillary (armpit) nodes. This is achieved via a combination of clinical examination, ultrasound. If an abnormality is found a biopsy will be performed. If there are no abnormalities, an additional screening test will be done at the time of surgery. This is called a sentinel lymph node biopsy and these results determine need for further surgery or radiotherapy. Treatment of breast cancer is complicated. It involves treatment for the breast, for the axilla and for potentially elsewhere in the body (if the cancer has spread). In patients whom the cancer has metastasized, treatments are mostly aimed at improving quality of life and comfort. Treatment strategies for breast cancer are outlined below and will be discussed in more detail during your consultation with Dr Edwina.
Treatment Options for Breast Cancer
a) Surgery
Treatment of your Breast Cancer will almost always involve surgery. Surgery is considered in two parts – surgery on the breast and surgery on the axilla (armpit).
Options for the breast are either a lumpectomy (removal of just the cancer) or a mastectomy (removal of the entire breast). Each option has unique advantages and disadvantages. If a lumpectomy is performed, a post operative course of radiotherapy is essential. Together the surgery and radiotherapy are termed ‘breast conservation’. If a mastectomy is performed, this may be combined with or without immediate reconstruction (by a plastic surgeon).
Axillary surgery is either a sentinel lymph node biopsy (when there is no clinical evidence of cancer in the armpit lymph nodes) or an axillary dissection (when there is evidence of cancer in the armpit lymph nodes). A sentinel lymph node biopsy is a diagnostic test, aiming to identify the first draining lymph node of the breast and whether there are cancer cells within it. Only a few lymph nodes are removed. By contrast, an axillary dissection is a therapeutic procedure, aiming to remove all the lymph nodes in the arm pit that the breast drains to.
b) Chemotherapy
Chemotherapy is anticancer or cytotoxic medication. Adjuvant chemotherapy is chemotherapy that is used after surgery to destroy any cancer cells that may have escaped into the bloodstream. The medical oncologist will look at the size of the tumour, the grade of the tumour, the number of lymph nodes involved, and the age of the patient in order to determine if chemotherapy is recommended. g the cancer more amenable to surgery and/or assessing its intrinsic aggressiveness.
Chemotherapy is anticancer or cytotoxic medication. Adjuvant chemotherapy is chemotherapy that is used after surgery to destroy any cancer cells that may have escaped into the bloodstream. The medical oncologist will look at the size of the tumour, the grade of the tumour, the number of lymph nodes involved, and the age of the patient in order to determine if chemotherapy is recommended.
There are many different chemotherapy regimens. Each has its unique indications.
It is usually an outpatient procedure and normally requires the patient to be in the hospital for a few hours on a single day. A chemotherapy session is termed a cycle and usually chemotherapy for breast cancer will be given in 4-6 cycles. Medication is given intravenously (as in infusion) and is relatively painless, but the treatment is exhausting and depending on which drugs are used there are several side effects ranging from minor to life threatening.
The most common side effect reported during chemotherapy is fatigue. Usually this will resolve after a few days’ rest. Other patients will have alterations in the way food smells and tastes, in addition to nausea and vomiting. Hair loss (alopecia) is also common. Some chemotherapy drugs can give sore mouth, mouth ulcers, or mouth infections, therefore oral hygiene is very important.
Chemotherapy can impact on fertility. This may be temporary or permanent. It is important that young women have a chance to see a fertility specialist before undergoing chemotherapy so that they can be given the opportunity to have eggs or embryos frozen before undergoing chemotherapy. It is also important that patients do not become pregnant during chemotherapy.
Some women will be able to work during their chemotherapy and others will not. A supportive workplace with flexible work hours is helpful and a doctor can always provide a medical certificate for patients that require time off.
c) Neoadjuvant chemotherapy (NAC)
Neoadjuvant therapy is essentially any treatment modality (chemo, endocrine, targeted therapy) which is given before surgery with the aim of making the cancer more amenable to surgery and/or assessing its intrinsic aggressiveness.
Historically, NAC was only offered to patients with locally advanced breast cancer (large, node positive, skin involvement or inoperable) or inflammatory breast cancer. However, it is increasingly common for patients with early stage breast cancer. Clinical trials have demonstrated the use of NAC is equivalent to adjuvant therapy in terms of overall survival. Where surgery treats the disease locally, chemotherapy has an effect on the whole body (systemic treatment). In pregnancy, NAC can buy time until delivery before proceeding to the surgery.
Assessment of the surgical specimen for residual tumour after NAC can provide powerful prognostic information. A complete pathological response (ie. no tumour present) is more likely seen to be seen in patients that have high grade ER negative and or HER-2 positive breast cancers compared to those that have low grade ER positive tumours. While neoadjuvant chemotherapy can have advantages, some patients may feel uncomfortable knowing the breast cancer is still in their body and therefore they may prefer to have surgery upfront. The pros and cons will be discussed with Dr Edwina during your consultation.
d) Endocrine Therapy
Patients who have Estrogen Receptor and Progesterone Receptor positive breast cancers may be offered endocrine therapy. The aim of endocrine therapy is to block intrinsic estrogen production, which is a driver for hormone positive breast cancer. Occasionally, patients with a high risk of breast cancer are treated prophylactically with endocrine therapy. The most common treatment regimens are selective oestrogen receptor modulators (e.g. Tamoxifen) which can be used in pre and postmenopausal women and aromatase inhibitors (eg. Anastrozole) which can only be used in post-menopausal women. Side effects of tamoxifen can include hot flushes, sweating, insomnia, and some sexual side effects such as a dry vagina and low libido. However recent studies have shown that 10 years of treatment with endocrine therapy is associated with an improvement in overall survival.
e) Targeted Cancer Therapy
HER2- positive breast cancers are more biologically aggressive compared to other breast cancer subtypes. Before the widespread use of Herceptin (Trastuzumab), overexpression of HER2 was associated with high recurrence rates and increased mortality. However, the use of Herceptin which is a monoclonal antibody which interferes with the HER-2/neu receptor and cell signalling has reversed this. Side effects of Herceptin include cardiac toxicity and therefore regular assessment is recommended during treatment.
f) Radiotherapy
The aim of radiotherapy is to kill cancer cells. Multiple studies have convincingly shown that radiotherapy reduces the risk of breast cancer recurrence. In patients with advanced disease who are not fit for surgery, it may be used as an alternative treatment. It is important for the surgical wound to be completely healed before radiation therapy is commenced. A planning session with a radiation oncologist is usually required, to determine the precise location to be targeted (which is tattooed). Standard treatment is daily (M-F) for several weeks. Short course radiotherapy is offered to some patient’s >50yrs. The machine which delivers the radiation is called a linear accelerator and is fairly noisy. The treatment itself is relatively painless although tiring and takes about 5 minutes. Many patients are able to continue with work whilst undertaking radiotherapy. It is important to realise that radiotherapy will not make you radioactive and it is quite safe for patients to go about their daily activities following treatment. They are absolutely no risks to close contacts of a patient undergoing radiotherapy, including children or babies.
Redness and blistering of the skin commonly occur in the third week. Other complications include sensory loss of the nipple, breast shrinkage (asymmetry), nausea, myalgia, inflammation of the lung and spontaneous rib fractures. An extremely rare but aggressive type of cancer is associated with breast radiotherapy, usually 5-10 years after completion of treatment.
A New diagnosis of Breast Cancer – things to know
The diagnosis of breast cancer is associated with many feelings, most commonly shock and denial at the diagnosis. Most breast cancers are asymptomatic, and patients do not feel unwell. Fortunately, the majority of breast cancers will be early breast cancers, which will have excellent outcomes. Tumour size and lymph node stage are diagnosis are the best predictors of outcome. Once the diagnosis is made, further investigations may be required, such as an MRI of the breast. Patients who present with large tumours (greater than 5 cm) or patients with known axillary lymph node metastasis will be asked to undergo preoperative CT staging in the form of CT scan of the chest, abdomen, pelvis, and a bone scan. All patients before surgery will undergo a full set of blood investigations and a chest x-ray. While the diagnosis of breast cancer may be a psychological emergency, it is not a surgical emergency.
When choosing a breast surgeon, it is important that not only is the surgeon technically competent (and can offer a wide variety of oncoplastic procedures) but is also supported by a multidisciplinary breast cancer team. The patient must also feel comfortable and have rapport with the treating surgeon.
- Do you specialise in breast cancer surgery?
- What will the surgery involve that is recommended for me?
- Where will the scars be placed and how will the breast look post-operatively?
- How long will I be in hospital?
- What is the expected recovery time?
- What are the risks of surgery and side effects of breast cancer treatment?
Multidisciplinary Care
There is good evidence that patients that have a multidisciplinary breast cancer team will have improved survival. The team consists of a breast surgeon, breast pathologist, medical oncologist, radiation oncologist, geneticist, breast radiologist and breast care nurses.
In general, patients with early breast cancers will proceed to surgery first, in order to remove the cancer and sample the lymph glands under the arm pit (sentinel lymph node biopsy). Following surgery, the pathology will be reviewed and together a need for any additional (adjuvant) treatment will be made eg. chemotherapy, endocrine therapy, targeted therapy and radiotherapy.
Pregnancy and Breast Cancer
Pregnant or breast-feeding women are not immune to breast cancer and these patients are faced with unique challenges. The treatment for breast cancer during pregnancy will depend on which stage of the pregnancy the breast cancer is diagnosed.
Pregnant or breast-feeding women are not immune to breast cancer and these patients are faced with unique challenges. The treatment for breast cancer during pregnancy will depend on which stage of the pregnancy the breast cancer is diagnosed.
- Breast imaging: it is safe to perform a breast ultrasound and biopsy during pregnancy. It is also possible to undergo a mammogram, although slightly uncomfortable and special precautions are usually adopted. MRI is not safe in pregnancy or lactation.
- Surgery: it is possible to undertake surgery at any stage of pregnancy however is ideally delayed until the second trimester or following delivery. Treatment options are the same, providing radiotherapy is permissible (if breast conservation is selected). Sentinel node biopsy is also acceptable during pregnancy , as only small doses of radioactive isotope injection are required.
- Radiotherapy: is not recommended during pregnancy but can be deferred until after delivery.
- Chemotherapy: should not be given during the first trimester (the time of organogenesis) but can be safely used thereafter. The risk of miscarriage or birth defect associated with chemotherapy in the 2nd and 3rd trimester is extremely low.
- Hormonal therapy/endocrine treatments: should be delayed until post-delivery. It is important for all women to understand all of their options carefully.
Nutrition and Exercise
Obesity is a known risk factor for many cancers, including breast cancer. The diet that is recommended following a diagnosis of or treatment for breast cancer, is the same as what is recommended for cancer prevention. Emphasis is placed on consuming a healthy and balanced diet, more so than adhering to any particular dietary regimes. A balanced diet refers to a diet that includes all nutrients necessary for your body’s normal function, and in adequate quantities to sustain a healthy weight or achieve weight loss. Adhering to a balanced diet means eating meals regularly throughout the day that consist of carbohydrates, protein and fats. There are no specific foods that should be consumed or avoided.
a) Calcium
Two to three serves of calcium-containing foods are recommended for most women per day in order to maintain bone health. Sample foods include low-fat dairy products (milk, cheese and yoghurt), canned salmon with edible bones, soy products (such as tofu and soymilk), almonds, brazil nuts and sesame seeds.
b) Alcohol
Studies have consistently shown that increased alcohol consumption is associated with an increase in the risk of breast cancer. For every standard drink (10g of alcohol) consumed daily, the risk of breast cancer has shown to increase by 7-12%. If women choose to consume alcohol, it is recommended that this is limited to one standard drink per day, a small glass of wine, and that they have multiple alcohol-free days per week.
c) Vitamin Supplements and ‘Anti-Cancer’ Diets
There is no scientific evidence that supports the use of vitamin supplements or any ‘anti-cancer’ diets (including herbal products) to prevent the recurrence of breast cancer. Dietary supplements are not equivalent to real food. A dietician or general practitioner may assist you when vitamin supplements are necessary.
d) Vitamin D
Vitamin D is essential for health and wellbeing. The recommended daily dose for maintenance is 2000IU/day. Vitamin D is sourced from the sunshine and food. Vitamin D deficiency has been associated with an increased risk of breast cancer.
e) Physical Activity
Regular exercise and a balanced diet are essential for maintaining a healthy weight and have also been shown to directly reduce the risk of 13 types of cancer. High levels of estrogen and insulin seen in obesity have been implicated in breast cancer development. Furthermore, obese and overweight patients are at increased risk of general surgical complications. It is recommended that all adults have at least two and a half hours of active physical exercise per week. This equates to 30 minutes five days per week. Exercise should be of moderate intensity, for example brisk walking or jogging and should be of sufficient intensity to make talking whilst exercising difficult. It is important to consume plenty of green leafy vegetables and fruits, complex carbohydrates, lean proteins, a moderate amount of dairy and small amount of healthy fats. Dr Edwina can explain this in more detail if you are curious.
Breast FAQs
- How long will I be in hospital after breast surgery?
This depends on the extent of surgery and your comfort afterwards. Typically patients undergoing a lumpectomy can go home the same day of surgery if they want to. For patients having axillary surgery (either a sentinel lymph node biopsy or an axillary dissection) it is advisable to stay at least overnight. For patients having a mastectomy, expect to stay 5-7nights. Dr Edwina Moore will review your progress in person every day that you are in hospital.
- What are the risks associated with breast surgery?
- Wound infection
- Hematoma (blood collection under the wound)
- Seroma (fluid collection under the wound)
- Need for re-excision of margins
- Hypertrophic or keloid scar (exaggerated scar)
- Arm Lymphedema (major arm swelling)
- Nerve injury
- Shoulder stiffness
- What is lymphedema?
Lymphedema refers to major limb swelling. It is most commonly caused by the removal of or damage to your lymph nodes as a part of cancer treatment. The risk of lymphedema after sentinel lymph node biopsy is very low and after axillary dissection is about 5-10%.
- Will I have a scar?
Yes. All incisions will heal with a scar. The aim is to perform a safe and appropriate operation, with the best cosmetic outcome (smallest, most discrete scar). Scars continue to remodel (and change in appearance) over 12months, up to 3 years. All patients heal (and therefore scar) differently. It is important to keep the wound clean, free from tension and covered from the sun. Dr Edwina will aim to place your scar either around the nipple or somewhere most cosmetically acceptable.
- When will I know the findings of the surgery?
Dr Edwina Moore will call your nominated support person immediately after surgery (while you are still drowsy) and given them an update. She will review you personally while in hospital. If at any stage you are uncertain, please ask. The final pathology report which requires meticulous study of the surgical specimen, usually takes one week and therefore will be available at the time of your post-operative review.
- Will I have stitches?
You will have some internal stitches that your body will absorb naturally. Your skin will be expertly closed with more absorbable stitches, medical glue and a ‘steri-strip’ (medical band-aid). There will be stitches that need removal. This technique ensures the best cosmetic outcome.
- Will I have any physical restrictions after my surgery?
In general, your activity level depends on the amount of discomfort you experience and the extent of surgery. Most patients return to work in a week or two, and you are able to drive as soon as your head can be turned comfortably without discomfort. For the best wound healing it is advisable not to perform any heavy activity (eg. lifting >7kg) for 4 weeks after surgery. It is also not advisable to bathe or swim with a fresh wound.
- What is the follow-up?
Following discharge from the hospital, Dr Edwina Moore will schedule a review consultation within 2 weeks. At this point, she will discuss any concerns of yours, the pathology, review your wounds and arrange any additional treatment if needed. Depending on the pathology you may need annual ongoing surveillance. Dr Edwina Moore will explain this to you during your appointment.