What is Colon & Rectal Cancer:
Colon and Rectal Cancer is the formation of cancer cells from the lining of the large bowel. Early diagnosis is associated with a better outcome, including cure. Timely review is critical!
Who is at risk:
Colorectal Cancer is the second most common cancer in women and third most common cancer in men. However, some people have a greater predisposition to developing cancer and may benefit from more frequent screening regimes.
Patients at greater risk are:
- Over the age of 50
- Have a personal history of colonic polyps
- Have a personal history of other cancers
- Have a personal history of inflammatory bowel disease
- Have a family history of Colorectal Cancers or polyps
- Have a known genetic condition that may predispose them to the development of cancers
What are the symptoms of Colon and Rectal Cancer:
Symptoms may depend on the location and size of the cancer. Most patients with early Colorectal Cancer do not have any symptoms.
Symptoms that alert medical practitioners are:
- Changes in bowel habit (an increased frequency of constipation and/or diarrhea)
- Change in stool consistency (toothpaste like)
- Blood mixed in with stool
- Weight lost, lethargy and/or anaemia
- Abdominal distension, bloating, vomiting and incomplete evacuation of stool.
How is Colorectal Cancer diagnosed:
A formal assessment includes taking a history, physical examination as well as a combination of blood and radiology tests. Specific tests that may be required include:
Colonoscopy:
This is the gold standard screening test of the large bowel for polyps and cancers. It also presents an opportunity to remove polyps and biopsy tumours that are too large to remove colonoscopically and send the tissue for microscopic analysis to provide a diagnosis and aid in further decision making.
Faecal Occult Blood test
This is a stool test that is sensitive for picking up blood in stool (which may be secreted by the cancer).
Radiology:
CT scan of the Chest, Abdomen and Pelvis is used to assess the size of the original (primary) cancer, and if it has spread to other organs.
MRI of the pelvis is used to assess the size of Rectal Cancers.

Image of the large bowel with a large ulcerated cancer in rectum. Depending on the size, these cancers can be asymptomatic, can bleed, cause pain or a bowel obstruction.
What is the treatment of Colorectal Cancer:
The main treatment of Colon and Rectal Cancer is surgical resection. In the majority of cases the segment of bowel effected by cancer is removed together with its blood supply and associated draining lymph nodes. I offer “keyhole” (laparoscopic/minimally invasive) surgery for all cancer resections, provided that this does not compromise the quality of the cancer surgery. Following resection, the two ends of bowel are joined together (anastomosis) whenever possible. I always try to avoid making a “stoma bag”, however, temporary and permanent stomas are sometimes required in Colorectal Cancer surgery.
Depending on the location and biology of the cancer a combination of Chemo and/or Radiotherapy may be required as part of your therapy. This may be before or after the surgical intervention.
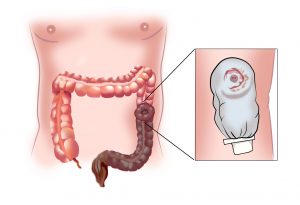
A stoma is an opening of the bowel onto the abdominal skin. This can be temporary or permanent depending on the patient’s condition. A stoma bag is an adhesive, scent free appliance that is placed around the stoma. Depending on the part of the bowel that is brought up the stoma can be on the right or left side of the abdomen.
Anal Cancer
What is Anal Cancer:
Cancerous cells may grow in the lining of the anal canal which is 3-4cm long and connects the anal opening to the rectum (bowel). The most common cell type in Anal Cancer is squamous cell carcinoma. Human Papilloma Virus (HPV) infections are attributed to causing Anal Cancer. Having HPV does not mean that the patient will go on to develop Anal Cancer, but it does increase the risk.
Who is at risk:
Anal Cancer is slightly more common in women than in men, and effects roughly 1 in 500-600 people.
Risk factors for Anal Cancer include:
- HPV infections.
- Multiple strains of HPV exist, and some of these strains are associated with cancers such as: anus, genitals, vulva, vagina, cervix, head and neck.
- Personal history of cancers associated with HPV (such as cervical)
- Personal history of “AIN” (anal intraepithelial neoplasia)
- Personal history of HIV infection or other immunocompromised condition
- Personal history of immunosuppression due to other medical conditions (such as organ transplants)
- Personal history of anal receptive sexual intercourse.
- Smoking history
- Over the age of 55
What are the symptoms of Anal Cancer:
Symptoms may depend on the location and size of the cancer. Most patients with early Anal Cancer do not have any symptoms.
Symptoms that alert medical practitioners are:
- Rectal bleeding, particularly when associated with bowel movement
- Anal pruritis (itch)
- Change in stool consistency (toothpaste like)
- Progressive faecal incontinence
- Anal pain
- Having a lump or an ulcer
- Feeling a constant need to go to the toilet “Tenesmus”
How is Anal Cancer diagnosed:
A formal assessment includes taking a history, physical examination as well as a combination of blood and radiology tests. Specific tests that may be required include:
Digital rectal exam:
The surgeon will inspect the anal area and than following application of lubricating jelly, will feel the anal canal with a gloved finger. This is performed with the patient awake.
Anal Papanicolau (Pap) Test:
This is a ‘Pap smear” test, just like for cervical cancer screening in women of appropriate age, but of the anal canal.
Biopsy:
Sometimes a small area of skin needs to be sent for microscopic analysis in the lab. The biopsy is typically performed under general anaesthesia in an operating theatre.
Radiology:
MRI of the perineum is used to assess the size of Anal Cancer.
CT scan of the Chest, Abdomen and Pelvis is used to assess if the Anal Cancer has spread to other organs.
What is the treatment of Anal Cancer:
The treatment of early Anal Cancers, that have not entered the anal wall may simply require a local excision. Bigger cancers are usually treated with a combination of Chemo and Radiotherapy. Chemoradiation is successful in the majority of patients, however the small percentage of patients that do not get an adequate response, or go on to have a recurrence (that is picked up on diligent follow up) require surgery. Major surgery for large or recurrent Anal Cancer requires an “abdominoperineal resection” (removal of rectum and anus) and formation of a permanent colostomy (stoma bag).
Rare tumours of Small and Large Bowel:
- Intestinal lymphoma
- Small bowel adenocarcinoma
- Neuroendocrine (carcinoid) tumours
- Gastrointestinal Stromal Tumours (GISTs)
- Presacral Tumours
- Appendiceal Neoplasms
These conditions are uncommon. Some patients are diagnosed with one of these conditions as part of investigations for a symptoms related to the gastrointestinal tract. Other patients are identified with an “incidental finding” when they are investigated for another condition.
Principles of assessment and management include:
- History and examination
- A biopsy to confirm the diagnosis
- Local staging to measure the size of tumour and involvement of adjoining organs
- MRI scan, Examination under Anaesthesia
- Systemic staging to see if the tumour has spread (metastasized) to other sites in the body
- CT chest, abdomen, pelvic and/or PET scan and blood tests
- Based on the above information a multidisciplinary discussion is held in a team of cancer specialists and a list of recommendations are then discussed with the patient and family. Typically, surgical resection if feasible offers the best chance of cure.
Familial Colorectal Neoplasia Screening:
Guidelines and databases
Up to 5% of all Colorectal Cancers are “hereditary”, which means that there is a known genetic mutation that can predispose such patients to develop a cancer, and that this mutation can be “inherited” from parent to offspring. Such patients require diligent follow up as specific mutations increase the risk of malignancy in other organs such as genitourinary system, breast, endocrine and gynaecological. Screening algorithms as well as prophylactic surgical interventions depend on the specific mutations. High risk patients are managed in conjunction with a genetic clinic and usually benefit from being linked to an international database.
In up to 20% of patients diagnosed with Colorectal Cancers, there may be a “familial” predisposition. Patients with a family history of Colorectal Cancer may have a higher risk of developing Colorectal Cancer, however unlike patients with “hereditary” Colorectal Cancer, do not carry an identified genetic mutation.
Further relevant information on familial and hereditary bowel cancer can be accessed via: www.cancer.org.au