Anatomy
The adrenal gland is a paired organ that sits at the back of the abdomen (the retroperitoneum) above the kidneys. For some reason, the adrenal glands are often overlooked. A normal adrenal gland is triangular in shape and about 2-3cm in size. The adrenal gland is made up of several layers. Each layer produces unique hormones which individually have several important functions. The outer cortex of the adrenal gland has three layers and the inner medulla has only one layer.
The adrenal glands can become diseased in three ways;
- Functional – produce excessive amounts of normal hormones
- Indeterminate – suspicion of cancer (large size, abnormal appearance, increase in size over time, personal history of other cancer)
- Cancer – primary which is related to the adrenal gland (adrenal cortical carcinoma) or secondary which has spread from elsewhere (metastatic)
Many patients with adrenal tumours (adenomas) have no symptoms at all and they are discovered incidentally from scans done for another reason. These tumours are termed ‘adrenal incidentalomas’. Other patients may present with symptoms related to a mass eg. discomfort. Patients with functional tumours can present with a variety of symptoms that are caused by hormone which is being secreted excessively.
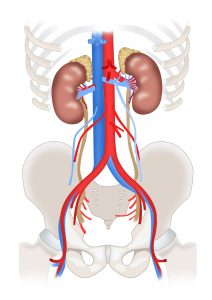
The adrenal gland is a paired organ that sits on top of the kidney, in the retroperitoneum.
Adrenal Incidentalomas
Adrenal incidentalomas are adrenal lesions ≥1 cm in size, identified serendipitously on imaging performed for unrelated indications. They are found in approximately 3% of abdominal CTs and the incidence has increased with increasing use and availability of scans. Overall, benign, non-functioning adrenal adenomas account for about 80% of adrenal incidentaloma. The aim of further evaluation is to determine whether a lesion may be hormonally active or potentially malignant, as this would affect future management decisions. Not all adrenal incidentalomas need surgery. Predictors of cancer are size and unique imaging characteristics. Dr Edwina Moore will explain more about this during your consultation.
Functional Adrenal Adenomas
Functional adrenal tumours are far less common than non-functional tumours, representing about 20% of adrenal incidentalomas. Patients may have symptoms related to the hormone excess or not (subclinical). Of the functional adrenal adenomas, pheochromocytomas and cortisol-producing are the most common, followed by aldosterone-producing tumours. Adenomas that produce sex hormones are extremely rare. Tumours may secret multiple hormones and this is highly suspicious of adrenal cancer.
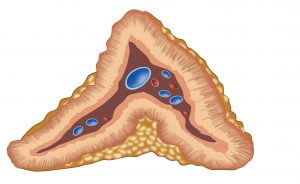
Each layer of the adrenal gland produces important and unique hormones that have variable physiological manifestations.
Aldosterone producing tumours (Conn’s Syndrome)
Primary aldosteronism is usually asymptomatic. The tumours are small and can be bilateral. Hallmarks of disease include uncontrollably high blood pressure and low potassium (hypokalaemia), although most patients with primary hyperaldosteronism actually have normal blood potassium (normokalaemia). Screening for primary hyperaldosteronism is recommended for patients with an adrenal mass who are hypertensive. A plasma aldosterone to plasma renin activity ratio is the recommended screening test. A plasma aldosterone concentration to plasma renin activity ratio of ≥20 is abnormal. Hyperaldosteronism can be caused by an adrenal adenoma or hyperplasia, which may be unilateral or bilateral. The distinction between the two entities is critical because management is entirely different (surgery vs medication). In patients greater than 40years, adrenal venous sampling is recommended to confirm which adrenal gland is producing excess hormone (laterality) as the tumour may not be big enough to see.
Cortisol producing tumours (Cushing’s syndrome)
Hypercortisolism may be asymptomatic but more often leads to vast array of signs and symptoms; central obesity, infertility, easy bruising, striae, poor wound healing, mood swings, osteoporosis, high blood pressure, high cholesterol and high blood sugar. It is important to ascertain whether the excess cortisol is coming from the adrenal gland (ACTH low) or pituitary (ACTH high). When the cortisol excess is due adrenal hypersecretion it is caused Cushing’s syndrome. Elevated 24-hour urinary cortisol levels are often a late finding in patients with Cushing’s syndrome. The recommended screening test is a 1mg dexamethasone suppression test, followed by a midnight salivary cortisol for confirmation. Treatment is surgical.
Phaeochromocytomas
These tumours produce excess hormones (catecholamines and metanephrines) that cause episodes of very high blood pressure and distinct spells characterised by severe headaches, excessive sweating, anxiety, palpitations and rapid heart rate. Such spells, left untreated, can result in life-threatening strokes or heart attacks. Pheochromocytomas may be related to a familial syndrome in which other endocrine organs are faulty (eg. MEN2, Von Hippel Lindau, neurofibromatosis and familial paraganglioma syndrome). Currently, there is no consensus as to the optimal biochemical screening test for these patients. Generally, we measure fractionated plasma metanephrines and 24-hour urinary catecholamines and it is important to cease medications such as tricyclic antidepressants and decongestants beforehand. Surgery, and in particular preparation for surgery, is highly complex and needs to be managed by a specialist endocrine surgeon.
Adrenal Cortical Cancer (ACC)
These are uncommon but highly aggressive cancers. They are often much larger at diagnosis (as they have been able to grow undetected) , causing symptoms related to size (mass effect). On imaging they have irregular margins and a generally abnormal appearance. Sometimes ACCs secrete multiple hormones concurrently. Urgent surgical referral is essential.
Adrenal Metastases
Less than 3% of incidental adrenal masses represent metastatic disease from another primary cancer, elsewhere in the body. Metastases to the adrenal gland are often bilateral. Provided that a pheochromocytoma has been excluded biochemically, biopsy may be performed to establish a diagnosis. Adrenal biopsy should be performed with utmost patient selection, if the results are suspected to change management.
Investigations and Indications for Adrenal Surgery
Once an adrenal mass has been identified, it is important to perform an appropriate workup to determine cause, essentially whether the tumour is functional (producing hormones) or cancer (either from the adrenal gland or elsewhere). This includes multiple blood tests, 24-hour urine collections and measurements and adrenal gland specific imaging (CT and MRI). Comparison of historical scans with contemporary scans is invaluable.
In general terms, the indications for surgery for an adrenal mass are;
- The tumour is found to make excess hormones
- The mass is large in size (more than 4cm in diameter) or has been shown to increase in size
- There is a suspicion for cancer
Adrenal FAQs
- How is an adrenal tumour removed?
You will be fully asleep with a general anaesthetic. There are 3 main approaches to surgery: open, keyhole (anterior) and keyhole (posterior also called retroperitoneoscopic). The decision is made after consideration of your individual scenario (BMI, body shape, existing scars, size and nature of the tumour). Sometimes, it is not possible to proceed with the original approach. The decision to convert from a keyhole procedure to an open procedure should not be viewed as a complication but a necessary decision to complete your operation safely. Once inside, the adrenal gland is dissected from the surrounding organs and fatty tissue. Major and minor vessels are sealed and divided, and then the gland is removed. Generally, patients who have open surgery require a longer stay in hospital because the incision is bigger but the long-term outcome is about the same.
- What should I expect after adrenal surgery?
Most patients can be cared for on the regular surgical ward after adrenal surgery. Sometimes patients with a phaeochromocytoma may go to an intensive care unit for extra monitoring (especially blood pressure). Many patients recover remarkably and are walking around the ward the day after surgery, Others can take a little longer to recover. It is important to remember that your body needs time to heal and adjust to being without the excessive hormone levels. You should expect a one-night stay in hospital, unless your medical condition requires that you stay longer. Patients with cortisol-producing tumours will need to take prednisone or cortisol pills temporarily after surgery. The dose will be tapered over time as the remaining normal adrenal gland regains normal function and secretes adequate cortisol hormone. Patients with aldosterone producing tumours can expect to gradually reduce their blood pressure medication following surgery.
- What are the potential complications of adrenal surgery?
The rate of major complications after PRA is less than 2%. Risks include:
- High blood pressure
- Bleeding
- Injury to surrounding organs eg. bowel, the liver on the right or the spleen or pancreas on the left.
- Infection of the incisions
- Bruising/swelling
- Incisional hernia (less common with PRA or laparoscopic surgery)
- Numbness or weakness of the muscles around the incision
- Collapsed lung (pneumothorax)
You will meet the anaethetist before your operation and will have the chance to ask any additional questions. Potential risks of the general anaesthetic include, but are not limited to:
- Heart problems (death, heart attack, arrhythmias)
- Lung problems (pneumonia, wheezing)
- Blood clots (stroke, clots in leg veins or lungs)
- Drug reactions (also possible with local anaesthetic)
- Chipped teeth
- Nerve pressure injuries
- Will I have much pain after surgery?
Most patients are surprised at how comfortable they are after laparoscopic (keyhole) surgery. Patients who have open surgery typically have more pain, although this can be managed with medication. You should be able to eat and drink normally, walk up and down stairs, and do light activity with relative ease almost immediately. Most patients take Panadol and/or Ibuprofen to keep them comfortable at home. This is sensible. You will have a prescription for something stronger for the first few days in case you need it, but beware prescription pain medicine can make you drowsy and constipated, so do not drive or operate heavy machinery, and drink lots of water and eat plenty of fruits and vegetables.
- When will I know the findings of the surgery?
The final pathology report requires careful study of the surgical specimen. Typically, this takes one week. We will discuss the pathology at the time of your post-operative review if not sooner.
- Will I have stitches?
You will have stitches on the inside that are naturally absorbed by the body after several weeks. You will also have a waterproof dressing covering the small incisions. You can shower with these but do not swim or bathe. Leave the dressing in place until your first post-operative visit, where it will be removed.
- Will I have any physical restrictions after my surgery?
In general, your activity level depends on the amount of discomfort you experience. Most patients return to work in a week or two, and you are able to drive as soon as you are comfortable (but not within 24hours of the general anaesthetic). Let your body be your guide and use your common sense. It is advisable not to perform any heavy lifting or straining exercises for at least 4 weeks as this can compromise healing of the muscles and result in an incisional hernia. You are not allowed to swim (spa or bath) for 4 weeks after surgery as this increases your risk of infection.
- What is the long-term follow-up after adrenal surgery?
This depends on the reason that you had surgery and Dr Edwina Moore will explain this to you in person during your consultation. Typically, she will see you within two weeks of surgery and at this time will discuss any concerns you have, your pathology results, check your wounds and arrange any additional treatment if necessary. Patients who have had functional adrenal tumours removed, require repeat blood and urine tests every year to assess for recurrence within the contralateral (opposite) adrenal gland.