Anatomy
The skin is composed of five layers: stratum coreneum, stratum lucidem, stratum granulosum, stratum spinosum and stratum basale. Below the skin is a layer of fat – subcutaneous fat (meaning below the skin), followed by fascia and then muscle.
There are many surgical pathologies that can affect the skin, including benign and malignant pathologies.
‘Lumps and bumps’ are causal names given to localized swollen areas that occur on or under the skin. There is a multitude of possible triggers including infection, a normal response to minor trauma or an abnormal proliferation of cells. Lumps and bumps are assessed by clinical examination and at times imaging studies. Depending on size, level of suspicion and location they can often be removed under local anaesthetic.
Benign tumours are non-cancerous and do not spread to other parts of the body. They can be removed surgically because they are unsightly or causing discomfort.
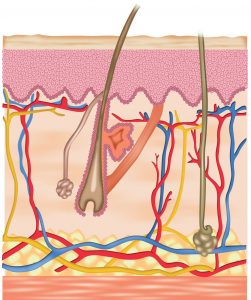
Cross-sectional view of the skin showing epidermis, dermis and subcutaneous fat.
Lipomas
Lipomas are slow growing, benign tumours that arise from fat cells. They are the most commonly occurring non-cancerous tumours in adults. Lipomas are soft or rubbery, round, usually mobile and can be found virtually anywhere in the body, especially on the shoulders, back or arms. They can develop at any age, often between 40 and 60 years of age. Treatment of lipomas is not essential but sometimes they may be painful or restricts the movement and simple excision is worthwhile. Surgical removal of a lipoma is very straight forward and involves a limited incision over the tumour and complete removal.
Sebaceous (epidermoid) cysts
A cyst usually is a slow-growing lump that can move easily under the skin. A sebaceous cyst is a closed sac found under the skin, usually on the trunk, neck, or face. They are filled with cheese-like matter and usually are painless. They may be caused by blocked a gland or swollen hair follicle. Sebaceous cysts are benign but they can enlarge and become infected. Treatment is surgery, ideally when they are not actively infected.
Lymph nodes
Lymph nodes are soft nodules of tissue that from a leading role in the lymphatic system, your body’s defence mechanism against infection. Lymph nodes help to identify germs and other foreign substances that invade our body. They are found throughout the body and may become swollen from infection, inflammation, infiltration or cancer. Enlarged lymph nodes are frequently found in the neck, armpit, under the jaw or chin, behind the ears and on the back of the head. They are diagnosed by physical examination assessing primarily for size, texture and tenderness. Where there is diagnostic uncertainty a biopsy may be performed. If lymph nodes are involved with cancer, they need to be removed along with the primary tumour.
Malignant tumours are cancerous tumours, that invade the surrounding tissue and spread to other parts of the body. They must be surgically removed .
Basal Cell Carcinoma (BCC)
This is the most common type of skin cancer and typically occurs on sun exposed skin. Historically it was called the ‘rodent ulcer’ because of its tendency to invade local structures. BCCs classically have a pearly edge and telangiectasia, but there are multiple different clinical subtypes. If there is diagnostic uncertainty in a cosmetically or functionally sensitive area, biopsy is recommended. Otherwise, the treatment is complete surgical excision.
Squamous Cell Carcinoma (SCC)
This is another common type of skin cancer, which may arise from premalignant lesions such as solar keratoses, chronic wounds/ulcers or de novo. Compared with BCCs, patients with SCCs are often older. They may appear as a crusted lesion with a classic everted edge. SCCs can spread to the lymph nodes, hence thorough examination of the regional basins (lymph draining sites) must be part of any examination. Treatment is surgery.
Melanomas
Melanomas are highly aggressive skin cancers which arise from melanocytes. One third of melanomas arise in pre-existing naevi (mole). The incidence of melanomas is rapidly increasing, which is alarming considering public education campaigns about the hazards of sun exposure. Classically melanomas are pigmented, but rarely they are amelanontic (not pigmented). We use the ABCDE rule when clinically assessing a potential melanoma – asymmetry, border irregularity, colour variegation, diameter (large) and elevation. However, the gold standard diagnostic test is excisional biopsy. Depending on multiple clinical and pathological factors, further treatment (including surgery) may be required. Dr Edwina will explain more about this if needed during your consultation.
Skin and soft tissue FAQs
- What are the some of the potential complications after skin and soft tissue surgery?
- Wound infection
- Hematoma
- Need for re-excision
- Recurrence
- Hypertrophic or keloid scar
- When will I know the findings of the surgery?
The final pathology report requires careful study of the surgical specimen. Typically, this takes one week. Dr Edwina Moore will discuss the pathology at the time of your post-operative review if not sooner.
- Will I have stitches?
You will have stitches on the inside (in the muscle) that are naturally absorbed by the body after several weeks. You will also have absorbable sutures in the skin. These do not need to be removed. A ‘steri-strip’ (medical band-aid) will cover your wound, offering protection and extra support. You can shower with this but do not swim or bathe. Leave the dressing in place until your first post-operative visit, where it will be removed.
- Will I have any physical restrictions after my surgery?
In general, your activity level depends on the amount of discomfort you experience. Most patients return to work after a few days, and you are able to drive as soon as you are comfortable (but not within 24hours of the general anaesthetic). Let your body be your guide and use your common sense. It is advisable not to perform any heavy lifting or straining exercises for at least 4 weeks as this can compromise healing.