Functional Bowel Disorders
Pelvic floor dysfunction
Pelvic floor muscles are a group of muscles in the pelvic area that support the pelvic organs including the rectum, bladder, and prostate/uterus. Pelvic floor dysfunction is the inability to coordinate the contraction and relaxation of muscles. This dysfunction may affect the evacuation of urine or stool.
Who is at risk:
The causes of pelvic floor dysfunction are multifactorial and difficult to isolate. Psychological trauma is frequently associated with pelvic floor dysfunction and in some cases the dysfunction is due to a learned behaviour (such as prolonged straining while on the toilet). Traumatic injuries to the pelvic area as well as vaginal childbirth have been associated with symptoms in some patients.
What are the symptoms:
A number of symptoms may be presents and need to be supplemented with an appropriate history and physical assessment of each patient. Some frequent symptoms include:
- Constipation or prolonged straining
- Inability to completely evacuate (tenesmus)
- Leakage of stool or urine without self-awareness
- Pelvic pain that may be aggravated by urination, defecation or sexual intercourse
How is Pelvic Floor dysfunction diagnosed?
A physical examination, including a digital rectal and vaginal exam is required at consultation. Most frequent radiological exams include:
- Endoanal ultrasound
- Anal Manometry
- Defecating proctogram
- Colonoscopy
- Examination of anus and rectum under anaesthesia (EUA)
What is the treatment of Pelvic Floor dysfunction?
Pelvic floor physiotherapy using biofeedback is helpful in over 75% of cases
Meditation and relaxation techniques such as yoga have been successful in some patients
Surgery including; injection of Botox to the pelvic musculature, or addressing causes of obstructive defecation such as rectocele or rectal prolapse are of benefit in selected cases
Faecal incontinence
Faecal incontinence can be defined as the inability to voluntarily control the release of stool or flatus until a socially appropriate time and place. The incidence of incontinence is difficult to measure due to the embarrassment associated with these symptoms. From population data in patients >45yo, up to 20% experienced an episode of faecal incontinence once per year, and 10% experienced an episode of faecal incontinence at least once per month.
As patients age, faecal incontinence becomes much more debilitating. It is the 2nd most common reason for admission to nursing home, making it more common than dementia.
Who is at risk:
The most common aetiology of faecal incontinence is associated with a history of sphincter injury (commonly childbirth trauma). However, men can also be affected and in the elderly the incidence of incontinence between men and women are equal.
Other causes may include reduction of pelvic muscle bulk due to aging, trauma, neuropathies, iatrogenic injury, connective tissue disorders and radiation injuries. A thorough medical assessment is essential to explore all causes of incontinence.
What are the symptoms:
Faecal incontinence is broadly divided into “urge incontinence” and “passive incontinence”. The reason for this is because the continence mechanism involves two types of muscles. The internal sphincter is a smooth muscle (similar to the heart or diaphragm, this muscle cannot be voluntarily activated). The external sphincter is a skeletal muscle and can be squeezed (flexed like the muscles in the arms or legs).
Symptoms are related to poor function in one or both of these muscles. Urge incontinence is the inability to squeeze the external anal muscle when the patient is experiencing an impending bowel movement. Passive incontinence is the low volume loss of liquid or gas due to the poor resting tone of the internal sphincter.
How is Faecal incontinence diagnosed?
A thorough history and examination are required. Important questions include;
- Frequency of episodes (daily, weekly, monthly)
- Whether incontinence is to solid, liquid stool or gas
- The amount of stool lost
- The need for continence pads and how frequently they need to be changed
- Usual bowel habits
- Specifically, history of chronic diarrhea
The use of a scoring system is helpful. We prefer using the Cleveland Clinic Continence Score.
Further investigations can be on muscle function (pelvic floor & anal sphincter), rectal compliance, sensory information, and stool consistency
Stool consistency: A patient with urgency and diarrhea is more likely to be incontinent. Therefore, it is important to perform a colonoscopy and exclude colonic inflammation (colitis) and mucous secreting polyps and cancers.
Rectal Compliance: A stiff, non-pliable rectum (for example due to a history of pelvic radiation) would precipitate urgency and place extra pressure on the pelvic floor muscles to maintain continence. This can be assessed either with a defecography study (under X-ray) or endoscopy.
Sphincter function and anorectal sensory information: This is termed “anorectal physiology” testing. It is a fairly short test performed in an anal manometry lab and involves a transducer and small rectal balloon catheter. The patient is awake for this test and it is typically well tolerated. A lot of useful information is derived from this and can aid management decision, however tests results do not necessarily corelate with pre-and post-operative incontinence scores. Particularly, measurement of pudendal nerve latency, a component of the test, is controversial.
Anal sphincter anatomy: Endoanal ultrasound is the most frequent test used for this. It can demonstrate a site and size of an anal sphincter defects. An MRI perineum may be an alternate test.
What is the treatment of Incontinence?
Faecal incontinence is a symptom complex, which may respond to conservative therapies. Surgery is an option when conservative management fails, or the symptoms are severe. A thorough workup is essential for successful management. New therapies are on the horizon, which will expand treatment options. Patient education as well as patient confidence is important to achieve an optimal outcome.
Medication and lifestyle modification are always commenced first. Pelvic floor physiotherapy, including “biofeedback” have been shown to significantly improve continence in a high proportion of patients. Barriers, such as anal plugs are useful in a particular patient demographic.
Surgical interventions are successful in selected patients. The best outcomes have been seen with Sacral Nerve Modulators-SNM (this is a neuroimplant, similar to a cardiac pacemaker). Biomaterial injections (to increase sphincter bulk) and sphincter repair can be of benefit in a limited number of patients.
Rectal prolapse
Rectal prolapse, also known as procidentia is the visible protrusion of the full thickness circular muscular folds of the rectum beyond the anal verge. Full thickness laxity of the rectum, which is internal, is termed “internal” rectal prolapse or rectal intussusception and is a condition that is treated differently from procidentia.
The condition is most common in elderly women with pelvic floor laxity and may co-exist with anterior organ prolapse (such as bladder and vagina). It is associated with incontinence in 50-75% of patients and therefore prolapse should be addressed prior to surgical intervention for faecal incontinence.
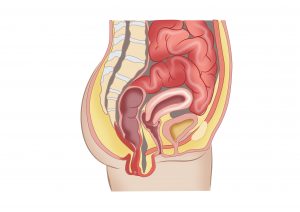
Transection of the female pelvis demonstrating the pelvic floor (bladder, vagina and rectum). When the rectum is “prolapsed”, the bowel hangs out of the anus.
Who is at risk:
Population statistics demonstrate that females are six times more likely to suffer from rectal prolapse than their male counterparts. The peak incidence is in females over the age of seventy with a history of multiple vaginal deliveries. Global weakness of the pelvic floor can predispose patients to rectal prolapse and therefore it is not infrequently seen in patients with urinary incontinence and vaginal prolapse, particularly following hysterectomy.
Young patients can also develop rectal prolapse. In this age group prolapse can be associated with congenital connective tissue disorders (such as Ehlers-Danlos syndrome). Other conditions that may predispose young patients to develop rectal prolapse include:
- GI dysmotility (slow transit constipation)
- Eating disorders
- Psychiatric comorbidities and development delay
What are the symptoms:
Due to the restrictions the condition may impose on activities of daily living, symptoms of rectal prolapse can be debilitating for patients and can render them homebound, isolated and depressed. Specific symptoms include:
Symptoms may include:
- Sensation of bulge during defecation that may require manual manipulation to “push back in”
- Mucous discharge
- Pelvic pressure and/or pain
- Rectal bleeding (particularly bright)
- Faecal accidents (including incontinence of solid, liquid or gas)
- Constipation and inability to evacuate completely (tenesmus)
How is rectal prolapse diagnosed:
Visual inspection of the prolapse is pathognomonic for this condition. The prolapse may appear spontaneously on straining, during the physical examination or require an examination under anaesthesia in a theatre environment. A screening colonoscopy is performed to exclude other conditions. Tests such as anal manometry, urodynamics studies and defecating proctogram may be used to evaluate other, associated pelvic floor conditions.
What is the treatment of Rectal prolapse?
Surgery is the only curative treatment of rectal prolapse, though it has been shown that Pelvic floor physiotherapy may improve post-operative function. Surgical approaches are broadly divided into abdominal and perineal. In broad terms a transabdominal repair has a reduced risk of recurrence, but a higher risk of complications.
Transabdominal Rectal Prolapse repair:
These procedures are based on “lifting the prolapse out of the pelvis” following entry into the abdominal cavity. These procedures can be performed in a minimally invasive approach (including Robotically). The specific procedure is tailored to the type of prolapse and fitness of the patient. The common procedures include:
- Ventral mesh rectopexy (including “Robotic Mesh rectopexy”)
- Laparoscopic Posterior rectopexy
- Resection Rectopexy
Perineal Prolapse repair:
The “Delorme” procedure (a mucosal sleeve resection) and an “Altemeier” procedure (resection rectosigmoidectomy) are the two types of repairs used vie the trans-anal approach. This approach involves delivering the prolapse out of the anus and either resecting it or stripping the mucosa and placating the muscle. These procedures are considered safer and may be performed under locoregional anaesthesia on very frail patients.